Corneal Ulcer: A - Z Guide
Definition
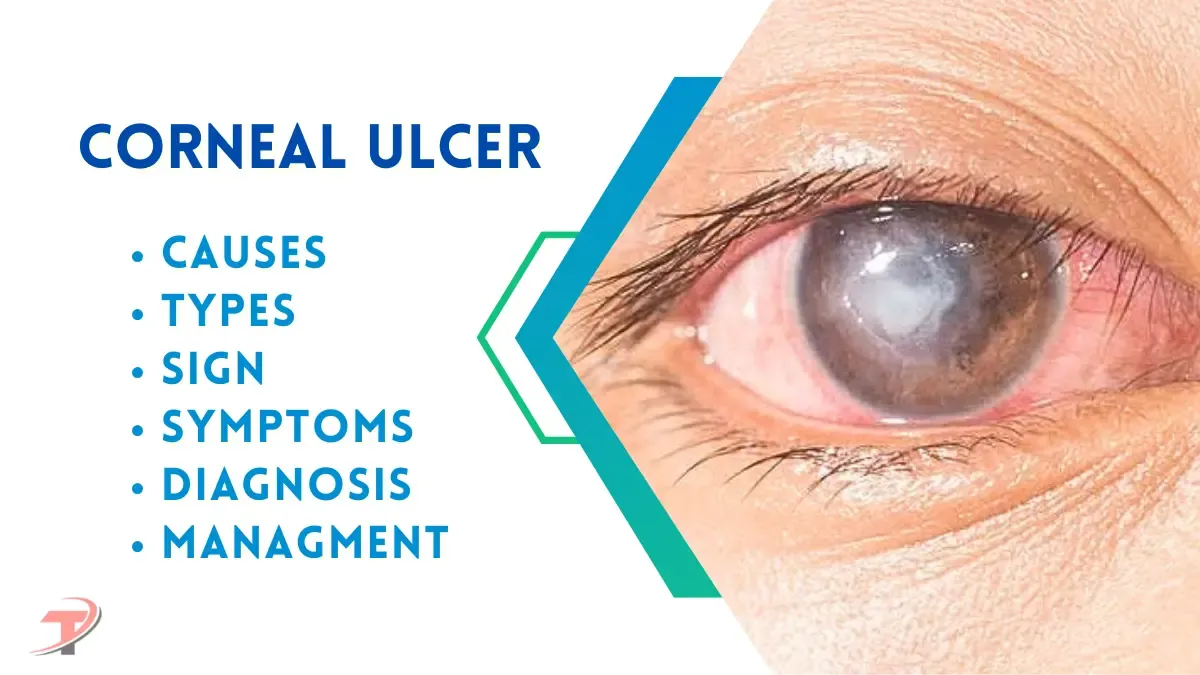
A corneal ulcer is an open sore or defect on the cornea, the clear, dome-shaped surface that covers the front of the eye. It often occurs due to an infection, trauma, or underlying eye condition. Corneal ulcers are a serious condition that can threaten vision if not promptly treated.
Types of Corneal Ulcers
1. Based on Etiology
- A. Infectious Corneal Ulcers
- Bacterial: Common organisms include Staphylococcus aureus, Pseudomonas aeruginosa, and Streptococcus pneumoniae. Features: Purulent discharge, hypopyon.
- Fungal: Common organisms include Aspergillus, Fusarium, and Candida. Features: Dry, feathery margins, satellite lesions.
- Viral:
- Herpes Simplex Virus (HSV): Dendritic or geographic ulcers, reduced corneal sensation.
- Herpes Zoster Ophthalmicus (HZO): Vesicular rash, pseudodendrites.
- Protozoal: Acanthamoeba. Associated with contact lens use, radial keratoneuritis.
- Chlamydial: Associated with trachoma and inclusion conjunctivitis.
- B. Non-Infectious Corneal Ulcers
- Neurotrophic Keratitis: Impaired corneal innervation, commonly due to HSV, diabetes, or trauma.
- Exposure Keratopathy: Inadequate lid closure, as seen in facial palsy or ectropion.
- Allergic or Immune-Mediated: Mooren's ulcer, peripheral ulcerative keratitis (PUK).
- Chemical or Toxic Injuries: From alkalis, acids, or drugs.
2. Based on Morphology
- Dendritic Ulcer: Seen in HSV infection.
- Geographic Ulcer: Enlarged dendritic ulcer, also in HSV.
- Ring Ulcer: Common in Acanthamoeba or fungal infections.
- Shield Ulcer: Associated with vernal keratoconjunctivitis.
- Peripheral Ulcer: Often seen in autoimmune conditions (e.g., rheumatoid arthritis).
3. Based on Depth
- Superficial Ulcer: Involves the epithelial layer only.
- Deep Ulcer: Extends into the stromal layer, may lead to perforation.
4. Based on Location
- Central Ulcer: Affects the visual axis, significant visual impact.
- Paracentral/Peripheral Ulcer: May occur due to systemic diseases or marginal keratitis.
5. Special Types
- Marginal Keratitis: Hypersensitivity reaction to staphylococcal antigens.
- Mooren's Ulcer: Idiopathic, painful, peripheral ulceration, often bilateral.
- Terrien’s Marginal Degeneration: Non-inflammatory thinning of the peripheral cornea.
- Interstitial Keratitis: Seen in syphilis, tuberculosis, or viral infections.
Causes
- Infections:
- Bacterial infections: Common in contact lens users.
- Viral infections: Herpes simplex virus (HSV) or varicella-zoster virus (shingles).
- Fungal infections: Often caused by plant material injury or in people using prolonged corticosteroids.
- Parasitic infections: Acanthamoeba, often associated with poor contact lens hygiene.
- Trauma: Eye injuries from foreign bodies, scratches, or chemical burns.
- Dry Eye Syndrome: Reduced tear production increases the risk of corneal damage and infection.
- Contact Lenses: Overuse, poor hygiene, or wearing them overnight.
- Underlying Conditions:
- Vitamin A deficiency.
- Eyelid disorders causing poor closure (e.g., lagophthalmos).
Signs and Symptoms
- Severe eye pain.
- Redness and swelling in the eye.
- Sensitivity to light (photophobia).
- Blurred or reduced vision.
- Discharge from the eye.
- A white or gray spot on the cornea visible to the naked eye.
- Excessive tearing.
- A sensation of a foreign body in the eye.
Diagnosis
- Clinical Examination: Using a slit lamp to assess the corneal lesion.
- Patient History: Noting recent trauma, contact lens use, or systemic illnesses.
- Fluorescein Staining: A dye is applied to the eye to highlight the ulcer under blue light.
- Culture and Sensitivity Tests: Samples from the corneal surface are analyzed to identify infectious agents.
- Additional Tests:
- PCR for viral causes.
- Confocal microscopy for parasitic infections.
Investigations
- Corneal scraping for microbial analysis.
- Complete blood count (CBC) to detect systemic infections.
- Tear film analysis for dry eye evaluation.
- Imaging: Ultrasound biomicroscopy if the view of the cornea is obscured.
Treatment
This is given for study purposes only for students. Patient should not use these medicines on self. If you are such a patient then please get treatment from your doctor.
1. Medical Management
- Bacterial Ulcers: Broad-spectrum antibiotics: Moxifloxacin, Ciprofloxacin, or Tobramycin.
- Fungal Ulcers: Natamycin 5% or Voriconazole drops.
- Viral Ulcers: Acyclovir ointment or oral Acyclovir (for herpes).
- Parasitic Ulcers: Polyhexamethylene biguanide (PHMB) or Chlorhexidine.
2. Supportive Treatment
- Cycloplegic eye drops (e.g., Atropine) to relieve pain and prevent complications.
- Artificial tears to maintain hydration.
3. Medications to Avoid
- Corticosteroids: Contraindicated in fungal and certain bacterial infections as they may worsen the condition.
Role of Vitamins
- Vitamin A: Essential for corneal health and epithelial repair. Deficiency can cause keratinization and ulcers.
- Vitamin C: Promotes collagen synthesis and aids in corneal wound healing.
Complications
- Corneal scarring leading to vision impairment.
- Perforation of the cornea.
- Endophthalmitis: Severe infection of the interior of the eye.
- Loss of the eye in extreme cases.
Management
1. Preventive Measures
- Practice good contact lens hygiene.
- Avoid eye trauma and foreign body exposure.
2. Surgical Options
- Corneal Transplant: In cases of severe scarring or perforation.
- Amniotic Membrane Grafts: For promoting healing in non-infectious ulcers.
3. Regular Follow-ups
- To monitor healing and prevent recurrence.
4. Patient Education
- Emphasize the importance of early treatment and adherence to therapy.